Insulin Resistance and Beyond: The Hidden Culprits
Sep 16, 2024
Aparna Hurtis
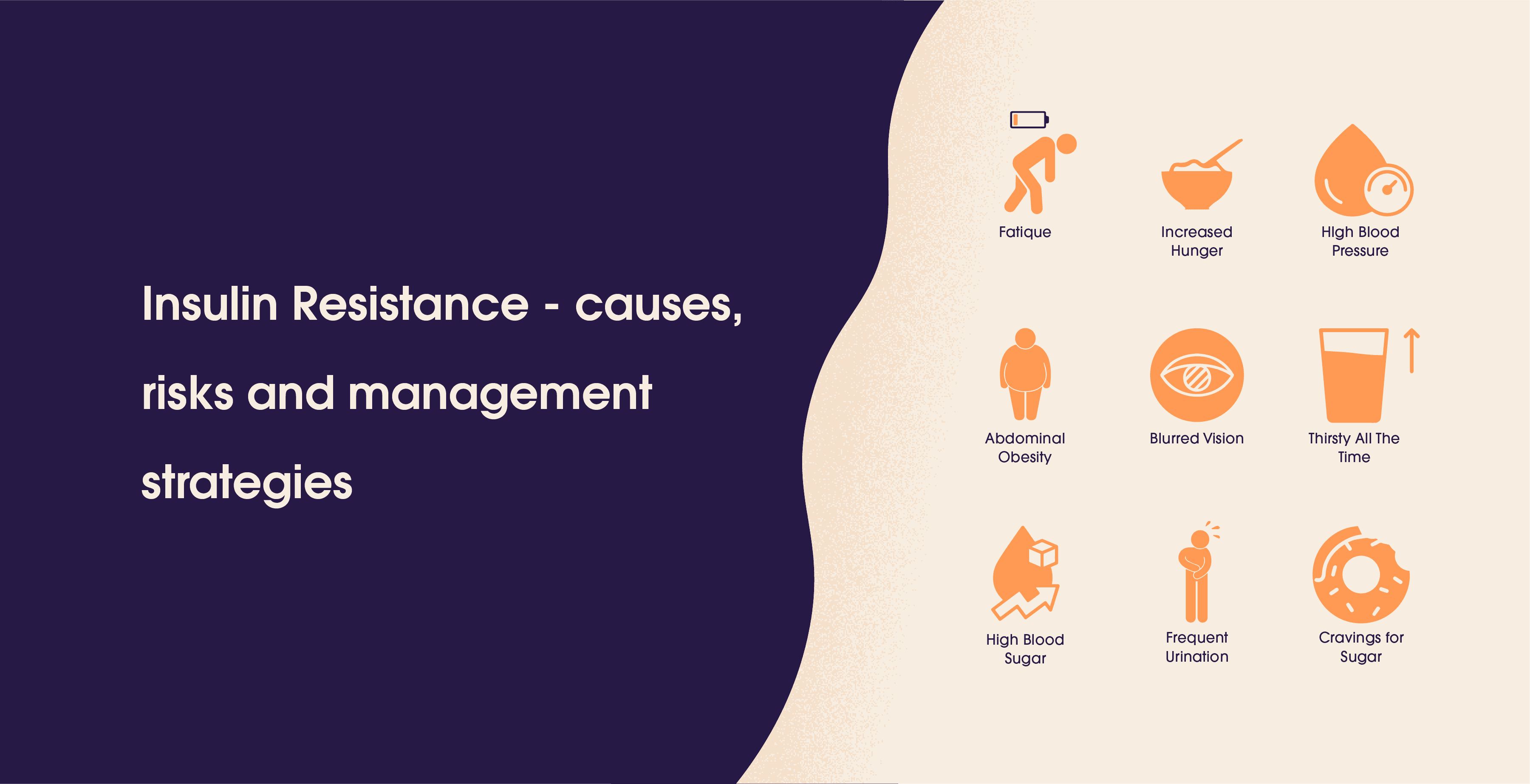
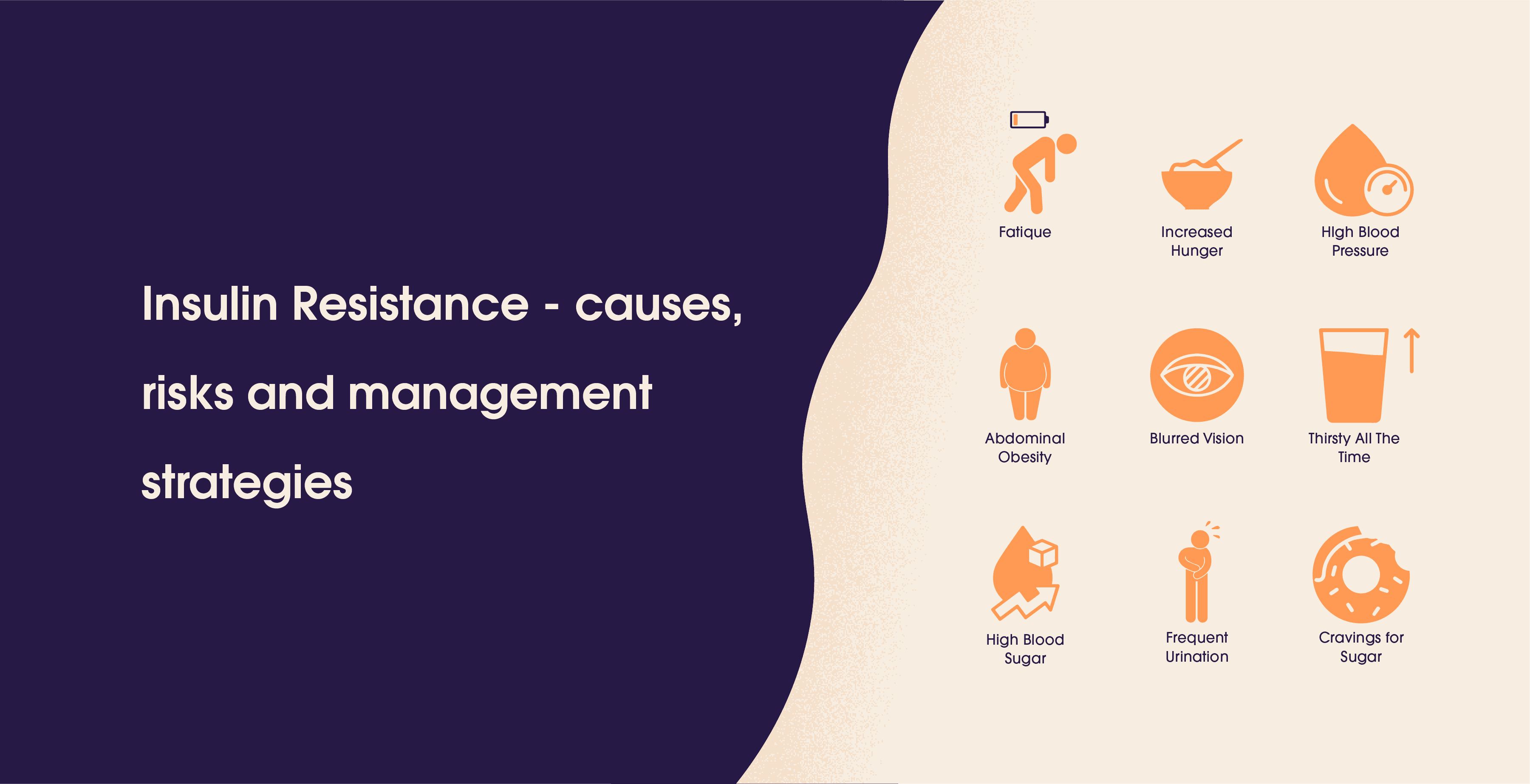
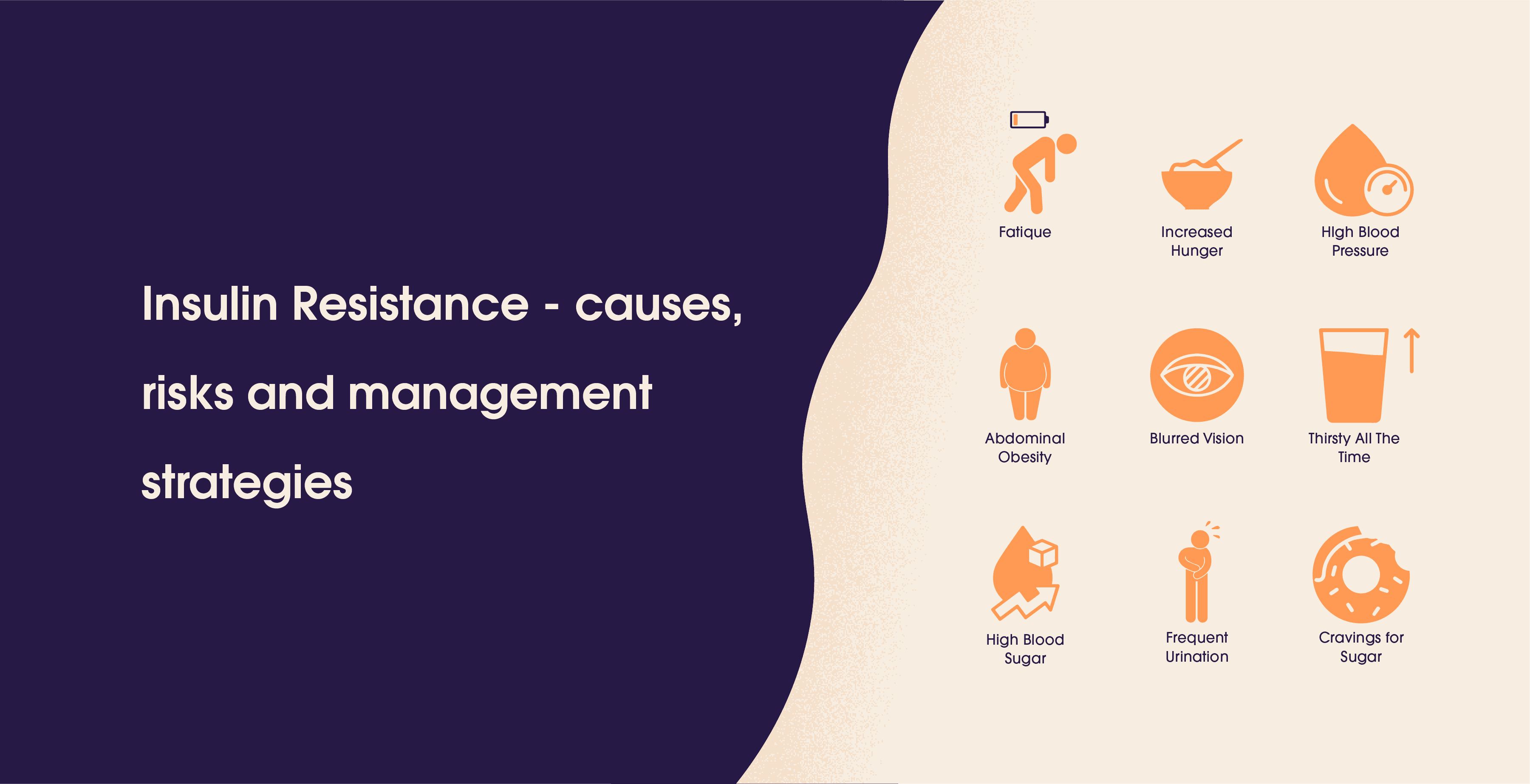
Table Of Contents
Insulin resistance, is a term that has been talked about a lot in the last couple of years be it a diagnosis for someone who is on the heavier side or for someone who has just gotten their PCOD/PCOS diagnosis. We have all heard the word, in this article, we will talk about insulin resistance and give you a comprehensive understanding of everything you need to know.
Highlights
Insulin is a hormone produced by the pancreas that helps convert sugar into energy.
Insulin resistance occurs when the body's cells don't respond properly to insulin, potentially leading to high blood glucose levels.
Causes include genetic factors, poor diet, lack of exercise, obesity, hormonal imbalances, chronic stress, and sleep disorders.
Common signs include fatigue, increased hunger, brain fog, dark skin patches, abdominal weight gain, and high blood pressure.
Diagnosis methods include HbA1c tests, fasting glucose tests, glucose tolerance testing, and sometimes random blood draws.
Untreated insulin resistance can lead to type 2 diabetes, cardiovascular diseases, PCOS, fatty liver disease, and metabolic syndrome.
Prevention strategies involve maintaining a healthy lifestyle, balanced diet, regular exercise, limiting alcohol, quitting smoking, and regular health check-ups.
Management and potential reversal include dietary changes, consistent exercise, medications, stress reduction, and improved sleep habits.
What is Insulin?
Before we jump into what insulin resistance is, it is necessary to understand what insulin is and what it does for our body. Insulin is a naturally occurring hormone in our body that is produced by the pancreas to help the body convert sugar into energy for our daily activities and needs.
What is Insulin Resistance?
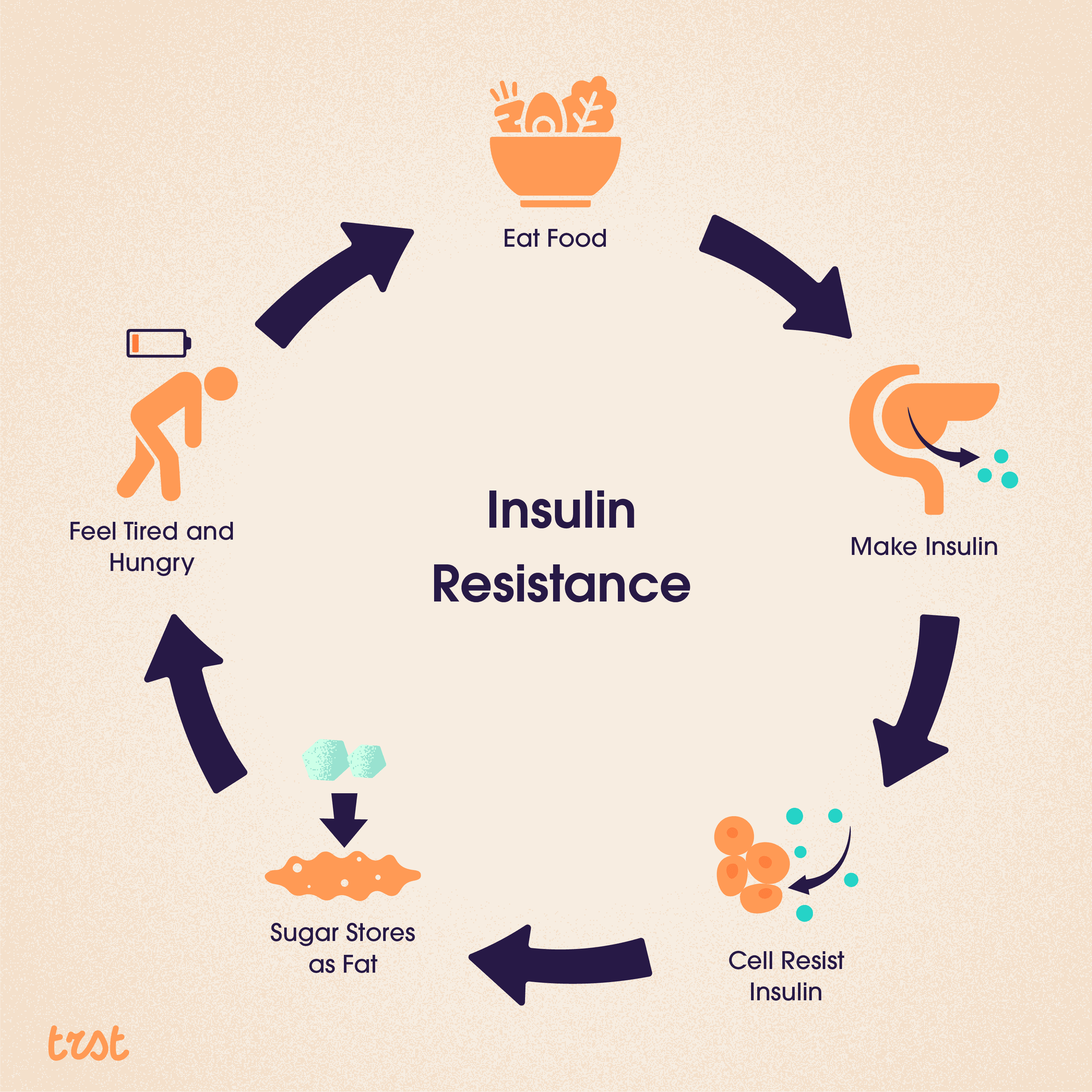
Now that we know what insulin is and what it does for our body, let’s understand what insulin resistance is, it is when our muscles, fat, and liver aren’t responding to the insulin as they should and are not able to completely take the glucose to function. This condition is called insulin resistance which can lead the body to have a spike in blood glucose levels. In some cases, insulin resistance is a temporary or short-term condition but if it is left untreated it can turn into diabetes.
Our main source of fuel is glucose, which we get when the food we eat breaks down. Once the glucose enters our bloodstream, insulin helps it get into our cells, even if it is used now or stored for later. That signals our pancreas to stop producing insulin.
But if you have insulin resistance then this process doesn’t work efficiently. Your cells aren’t absorbing the glucose when insulin asks them to. As a result more and more glucose piles up in your bloodstream, and your pancreas keeps making insulin.
For a while making the extra insulin will be possible for the pancreas, which will help keep your glucose levels in the normal range but over time, your cells may become more insulin resistant causing your blood glucose levels to rise.
Difference Between Insulin Resistance and Diabetes
The first thing we need to understand is that anyone can develop insulin resistance either temporarily or chronically, and like any other disease over time chronic insulin resistance can lead to pre-diabetes that converts into Type 2 diabetes if it is not treated.
The bridging condition between insulin resistance and type 2 diabetes is pre-diabetes, this is a condition where your blood glucose levels are higher than normal but not high enough to be diagnosed with diabetes. Pre-diabetes happens in people who already have some level of insulin resistance.
Insulin resistance isn’t diabetes but a heightened condition that happens to a person when their pancreas can no longer make enough insulin, resulting in high blood glucose levels.
What Causes Insulin Resistance?
Now that we know the difference, let’s understand what are the causes of Insulin resistance - it is a combination of various factors -
Genetic Factors
Your genes play a significant role in determining your vulnerability to insulin resistance. Some of us are genetically predisposed to this condition, making us more likely to develop insulin resistance even with a healthy lifestyle.
Lifestyle Factors
These are often the most significant contributors. -
Diet: A diet high in processed food, sugars, and unhealthy fats can lead to insulin resistance
Exercise: Low physical activity reduces our body's ability to use insulin effectively.
Obesity: Excess body fat, especially around the abdomen, is strongly linked to insulin resistance.
Other Factors: Other than our lifestyle and genetic factors there are a few more contributing factors:
Hormonal Imbalance: Conditions like PCOS can increase the risk of insulin resistance.
Medication: Some medications can interfere with insulin sensitivity.
Chronic stress: High levels of stress hormones (cortisol) can impair insulin function.
Sleep disorders: Poor sleep quality or quantity can affect insulin sensitivity.
It is necessary to understand these factors as they will help you prevent and manage insulin resistance.
What are the Signs of Insulin resistance?
There are many signs that we experience in our daily lives but are unaware of how to recognize them, and recognizing the signs is vital for early detection and treatment. These are the most common symptoms -
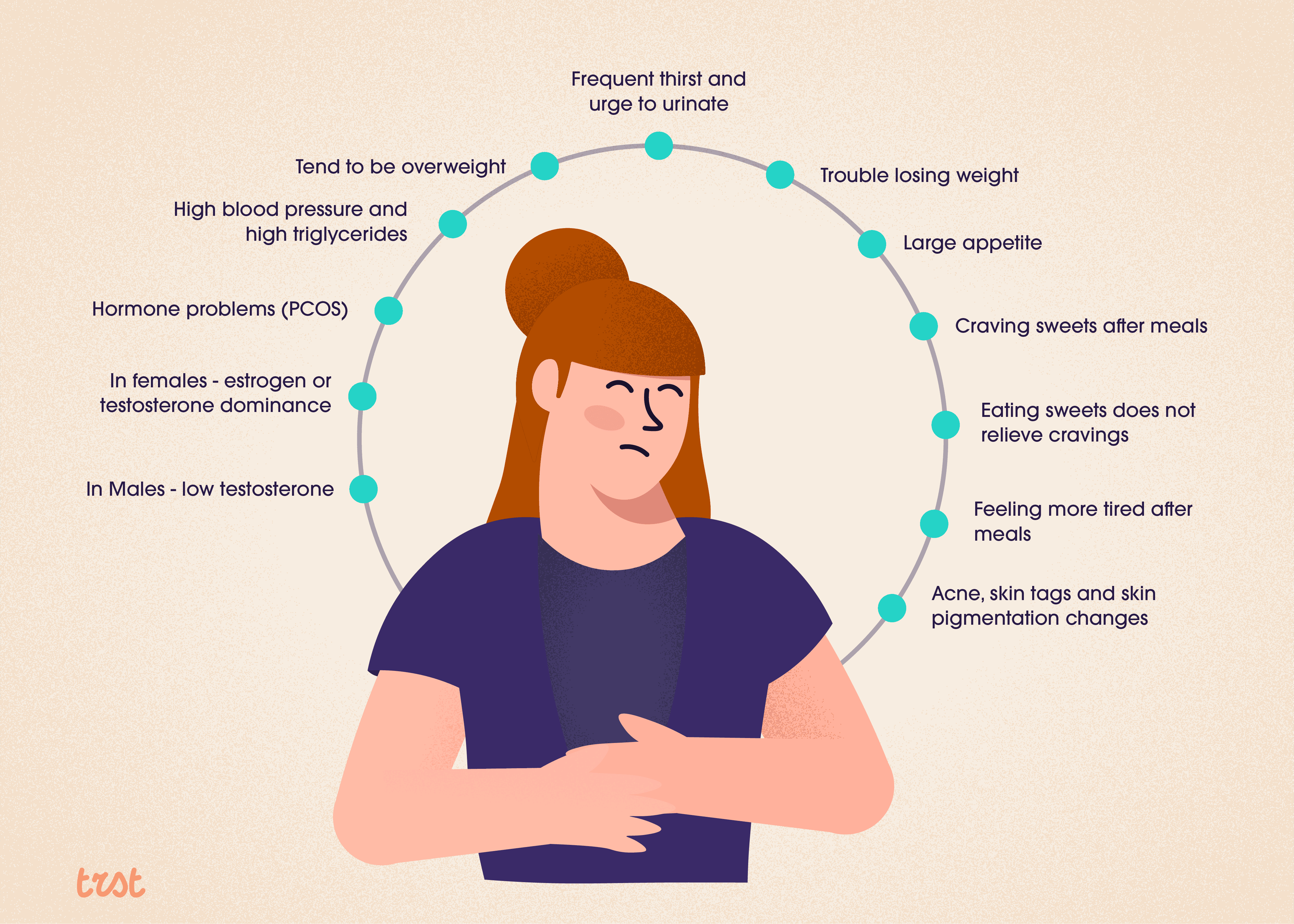
Other common signs are -
Fatigue: Feeling tired, especially after meals
Increased hunger: Craving food, particularly carbs.
Brain Fog: Having difficulty concentrating or trouble focusing.
Dark Patches of skin: Known as Acanthosis nigricans, appear on the neck, armpits, or groin.
Weight gain: Especially around the abdomen.
High blood pressure: Often associated with insulin resistance.
It is important to note that, many of us do not experience noticeable symptoms in the early stages. It is advised to get regular check-ups and blood tests for early detection. If you are experiencing any of these symptoms or have risk factors, consult your healthcare provider.
How To Diagnose Insulin Resistance?
There are multiple ways to diagnose insulin resistance. Your doctor will ask you about your symptoms, family history, and lifestyle. They’ll also check your weight, and blood pressure, and look for physical signs like acanthosis nigricans. Here are some of the tests that help in diagnosing insulin resistance -
HbA1c test
The A1c test is one way to diagnose insulin resistance, prediabetes, and diabetes. This test measures the average of your blood sugar over the previous 2 to 3 months.
Generally classified here are what the results mean:
An HbA1c under 5.7 % is considered normal
An HbA1c between 5.8 to 6.4% is considered prediabetic
An HbA1c equal to or above 6.5% is diagnosed as diabetes.
You’ll need your doctor to reconfirm the results. However, depending on the lab you have chosen for the test, the numbers could vary by 0.1% to 0.2%.
Fasting Glucose Test
This test shows your fasting blood sugar levels. For this test, you are required to fast (not eat or drink anything) for at least 8 hours. Your Doctor will be able to make a diagnosis for prediabetes or diabetes using this test.
Generally, here is what the results mean:
Fasting blood sugar levels under 10mg/dL is considered normal
Levels between 100 and 125 mg/dL are diagnostic for prediabetes
Levels equal to or greater than 126 mg/dL are diagnostic for diabetes.
Depending on the lab, these numbers can vary up to 3 mg/dL points in the cutoff numbers.
Glucose Tolerance Testing
A 2-hour glucose tolerance test is another way of diagnosing prediabetes or diabetes. Your blood glucose levels are taken before the test after which you will be given a premeasured sugar drink, and your blood glucose levels are checked again in 2 hours.
Generally, here’s what the results mean:
A blood glucose level under 140 mg/dL after 2 hours is considered normal.
A blood glucose level between 140 and 199 mg/dL is considered prediabetes.
A blood glucose level of 200 mg/dL or higher is considered diabetes.
Random Blood draws
Random blood sugar tests are useful if you are experiencing significant diabetes symptoms. However, the ADA ( American Diabetes Association) does not recommend random blood glucose tests for routine diabetes screening or the identification of pre-diabetes.
In Addition to all these tests, your doctor may also check your cholesterol levels, as insulin resistance often occurs alongside dyslipidemia (a metabolic disorder that occurs when there are abnormally high or low levels of lipids or lipoproteins in the blood.)
What are the Risks of Ignoring Insulin Resistance?
Insulin resistance if ignored can lead to a lot of serious health complications like -
Type 2 Diabetes - Insulin resistance is a known precursor to type 2 diabetes and without intervention, you have a higher chance of developing diabetes in the next 10 years.
Cardiovascular Diseases - Insulin resistance is associated with a higher risk of heart disease, and stroke due to its effects on blood pressure, cholesterol levels, and inflammation.
Polycystic Ovary Syndrome (PCOS/PCOD) - Insulin resistance can heighten hormonal imbalance in women.
Non-Alcoholic Fatty Liver Disease - With insulin resistance, and the body not being able to process excess glucose, it deposits as a fat layer on the liver causing fatty liver.
Metabolic Syndrome - A cluster of conditions like high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels are also associated with insulin resistance.
Early intervention and management are very crucial in preventing serious health risks.
Can Insulin Resistance Be Prevented?
While insulin resistance can be prevented in some cases, the genetic risk factors can’t be changed but there is good news! Many strategies can help prevent insulin resistance:
Living a healthy lifestyle: Adopting a healthy lifestyle is the cornerstone of prevention. This means maintaining a healthy weight, eating a balanced diet, and staying physically active.
Balanced Diet: Focus on whole foods, lean proteins, healthy fats, and complex carbohydrates.
Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise per week.
Healthy weight: Keep your BMI within the healthy range.
Limit alcohol and Quit Smoking: Alcohol and smoking can contribute to insulin resistance.
Monitoring risk factors: Regular check-ups and blood tests can help identify early signs of insulin resistance. If you have risk factors like a family history of diabetes or obesity, more frequent monitoring may be recommended.
How can Insulin Resistance Be Managed or Reversed?
The answer to this is yes it can be managed or reversed. Managing the condition often involves lifestyle changes and in some cases medication:
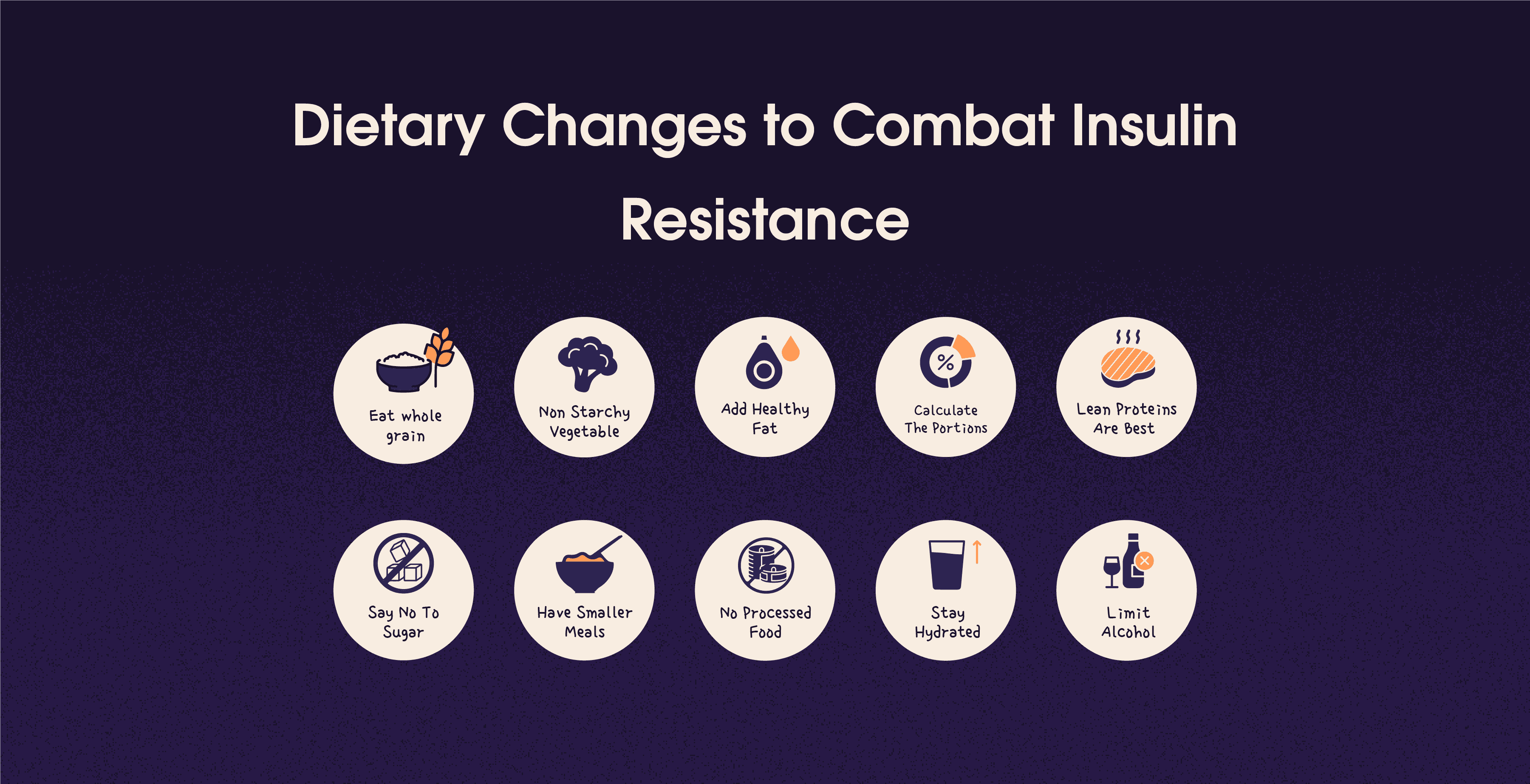
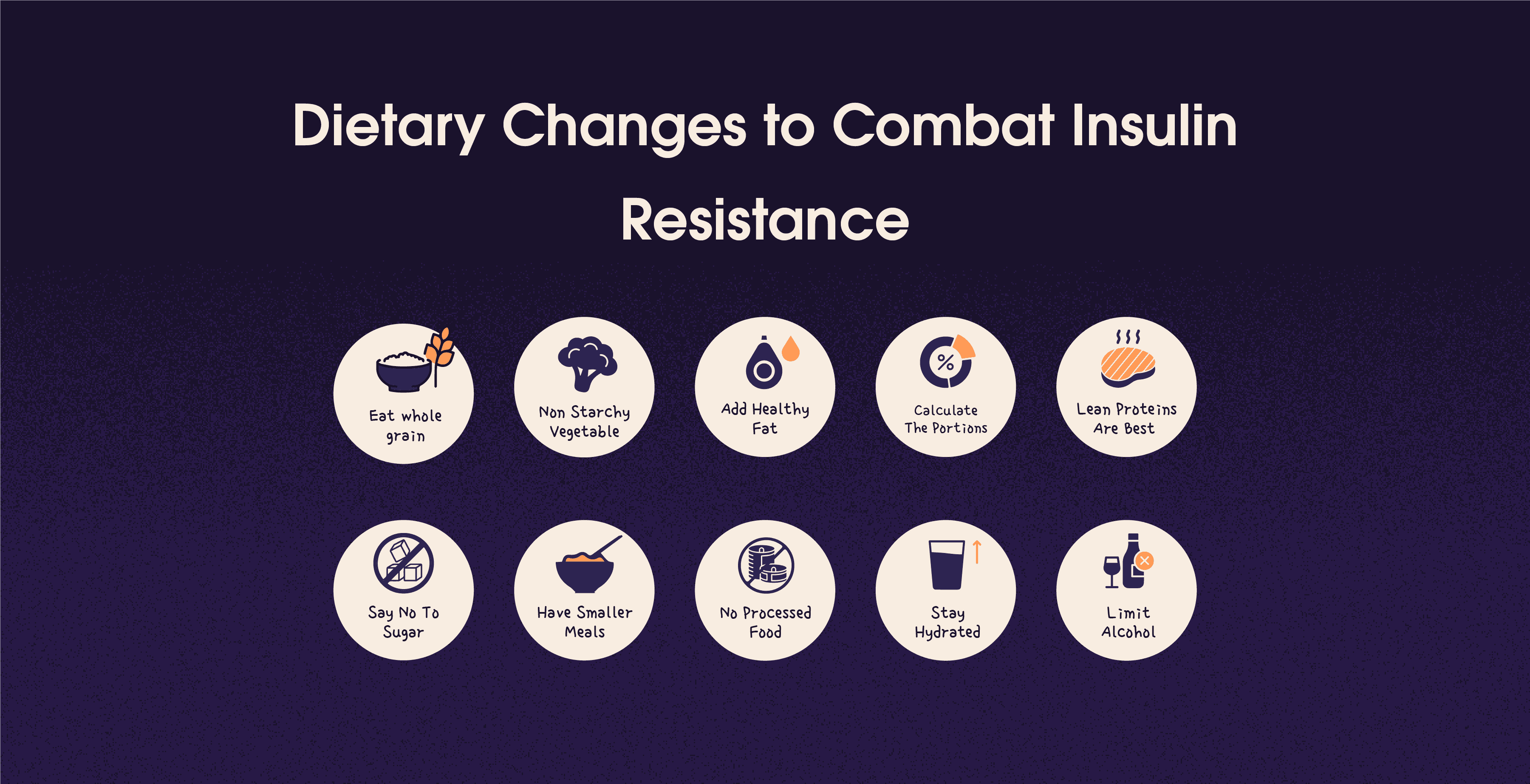
Dietary Changes
Low-carb diets: Reducing carb intake, especially refined carbs, can improve insulin sensitivity.
Increased Fiber: A high-fiber diet helps regulate blood sugar levels.
Reducing sugar intake: Limit added sugar and sweetened beverages.
Healthy fats: Incorporate sources of omega-3 fatty acids and monounsaturated fats.
Exercise
Aerobic exercise: Regular cardio activities like walking, swimming, or cycling.
Resistance training: Strength training helps build muscle, which improves insulin sensitivity.
High-intensity interval training (HIIT) can be particularly effective for improving insulin function.
Medication and Supplements
Metformin: A common medication that can improve insulin sensitivity.
Omega-3 Fatty acids: These may help you reduce inflammation and improve insulin function.
Berberine: A supplement that has shown promise in improving insulin sensitivity.
Lifestyle Modification
Stress reduction: Practice meditation, yoga, or deep breathing exercises to help with stress.
Sleep!: Aim for 7-9 hours of quality sleep a night to help with insulin resistance.
Weight Loss: Modest weight loss can significantly improve insulin sensitivity.
Conclusion
Insulin resistance is a serious condition that leads to significant health complications if left unmanaged. However, with early detection and appropriate lifestyle changes, it is possible to improve, manage and reverse insulin resistance.
Insulin resistance, is a term that has been talked about a lot in the last couple of years be it a diagnosis for someone who is on the heavier side or for someone who has just gotten their PCOD/PCOS diagnosis. We have all heard the word, in this article, we will talk about insulin resistance and give you a comprehensive understanding of everything you need to know.
Highlights
Insulin is a hormone produced by the pancreas that helps convert sugar into energy.
Insulin resistance occurs when the body's cells don't respond properly to insulin, potentially leading to high blood glucose levels.
Causes include genetic factors, poor diet, lack of exercise, obesity, hormonal imbalances, chronic stress, and sleep disorders.
Common signs include fatigue, increased hunger, brain fog, dark skin patches, abdominal weight gain, and high blood pressure.
Diagnosis methods include HbA1c tests, fasting glucose tests, glucose tolerance testing, and sometimes random blood draws.
Untreated insulin resistance can lead to type 2 diabetes, cardiovascular diseases, PCOS, fatty liver disease, and metabolic syndrome.
Prevention strategies involve maintaining a healthy lifestyle, balanced diet, regular exercise, limiting alcohol, quitting smoking, and regular health check-ups.
Management and potential reversal include dietary changes, consistent exercise, medications, stress reduction, and improved sleep habits.
What is Insulin?
Before we jump into what insulin resistance is, it is necessary to understand what insulin is and what it does for our body. Insulin is a naturally occurring hormone in our body that is produced by the pancreas to help the body convert sugar into energy for our daily activities and needs.
What is Insulin Resistance?
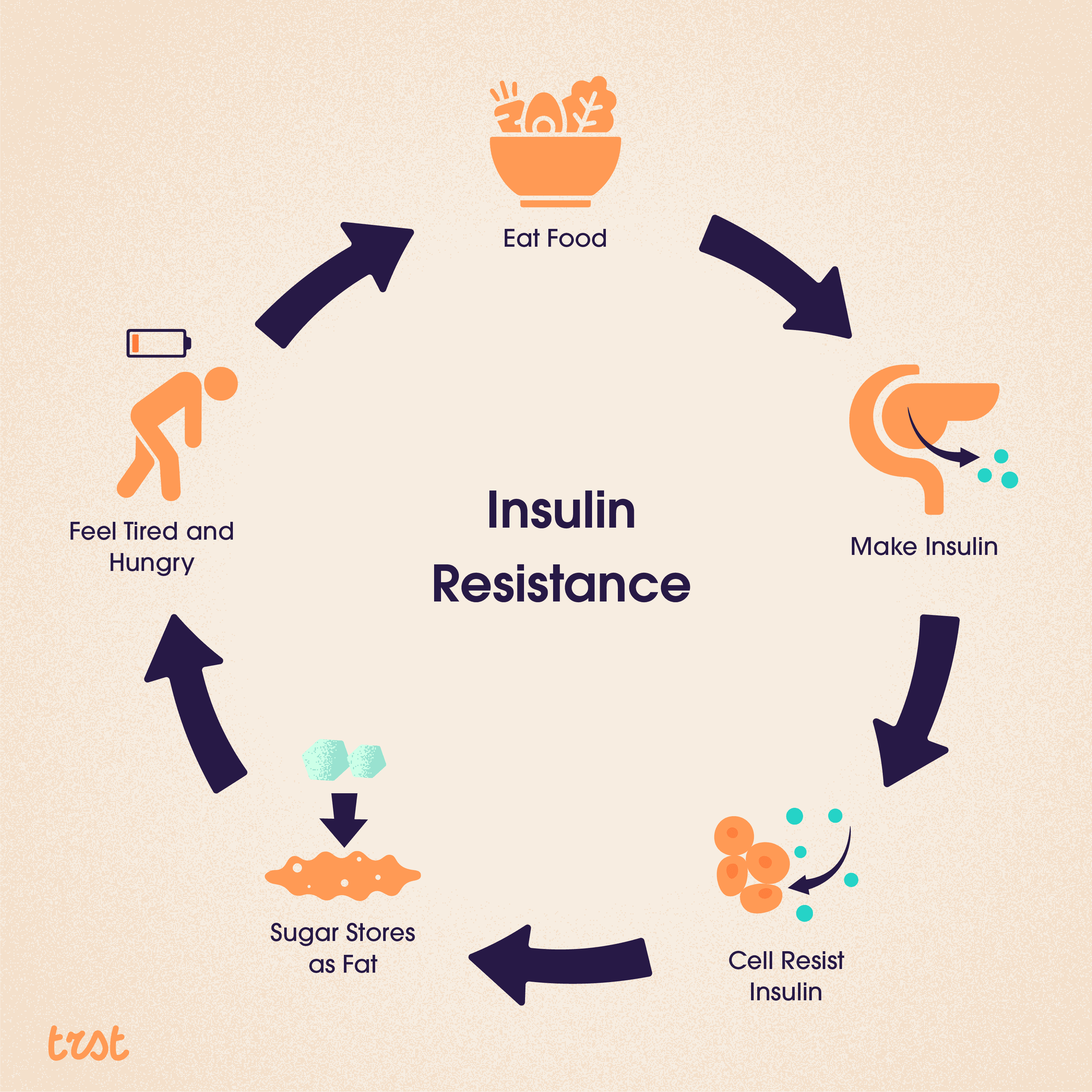
Now that we know what insulin is and what it does for our body, let’s understand what insulin resistance is, it is when our muscles, fat, and liver aren’t responding to the insulin as they should and are not able to completely take the glucose to function. This condition is called insulin resistance which can lead the body to have a spike in blood glucose levels. In some cases, insulin resistance is a temporary or short-term condition but if it is left untreated it can turn into diabetes.
Our main source of fuel is glucose, which we get when the food we eat breaks down. Once the glucose enters our bloodstream, insulin helps it get into our cells, even if it is used now or stored for later. That signals our pancreas to stop producing insulin.
But if you have insulin resistance then this process doesn’t work efficiently. Your cells aren’t absorbing the glucose when insulin asks them to. As a result more and more glucose piles up in your bloodstream, and your pancreas keeps making insulin.
For a while making the extra insulin will be possible for the pancreas, which will help keep your glucose levels in the normal range but over time, your cells may become more insulin resistant causing your blood glucose levels to rise.
Difference Between Insulin Resistance and Diabetes
The first thing we need to understand is that anyone can develop insulin resistance either temporarily or chronically, and like any other disease over time chronic insulin resistance can lead to pre-diabetes that converts into Type 2 diabetes if it is not treated.
The bridging condition between insulin resistance and type 2 diabetes is pre-diabetes, this is a condition where your blood glucose levels are higher than normal but not high enough to be diagnosed with diabetes. Pre-diabetes happens in people who already have some level of insulin resistance.
Insulin resistance isn’t diabetes but a heightened condition that happens to a person when their pancreas can no longer make enough insulin, resulting in high blood glucose levels.
What Causes Insulin Resistance?
Now that we know the difference, let’s understand what are the causes of Insulin resistance - it is a combination of various factors -
Genetic Factors
Your genes play a significant role in determining your vulnerability to insulin resistance. Some of us are genetically predisposed to this condition, making us more likely to develop insulin resistance even with a healthy lifestyle.
Lifestyle Factors
These are often the most significant contributors. -
Diet: A diet high in processed food, sugars, and unhealthy fats can lead to insulin resistance
Exercise: Low physical activity reduces our body's ability to use insulin effectively.
Obesity: Excess body fat, especially around the abdomen, is strongly linked to insulin resistance.
Other Factors: Other than our lifestyle and genetic factors there are a few more contributing factors:
Hormonal Imbalance: Conditions like PCOS can increase the risk of insulin resistance.
Medication: Some medications can interfere with insulin sensitivity.
Chronic stress: High levels of stress hormones (cortisol) can impair insulin function.
Sleep disorders: Poor sleep quality or quantity can affect insulin sensitivity.
It is necessary to understand these factors as they will help you prevent and manage insulin resistance.
What are the Signs of Insulin resistance?
There are many signs that we experience in our daily lives but are unaware of how to recognize them, and recognizing the signs is vital for early detection and treatment. These are the most common symptoms -
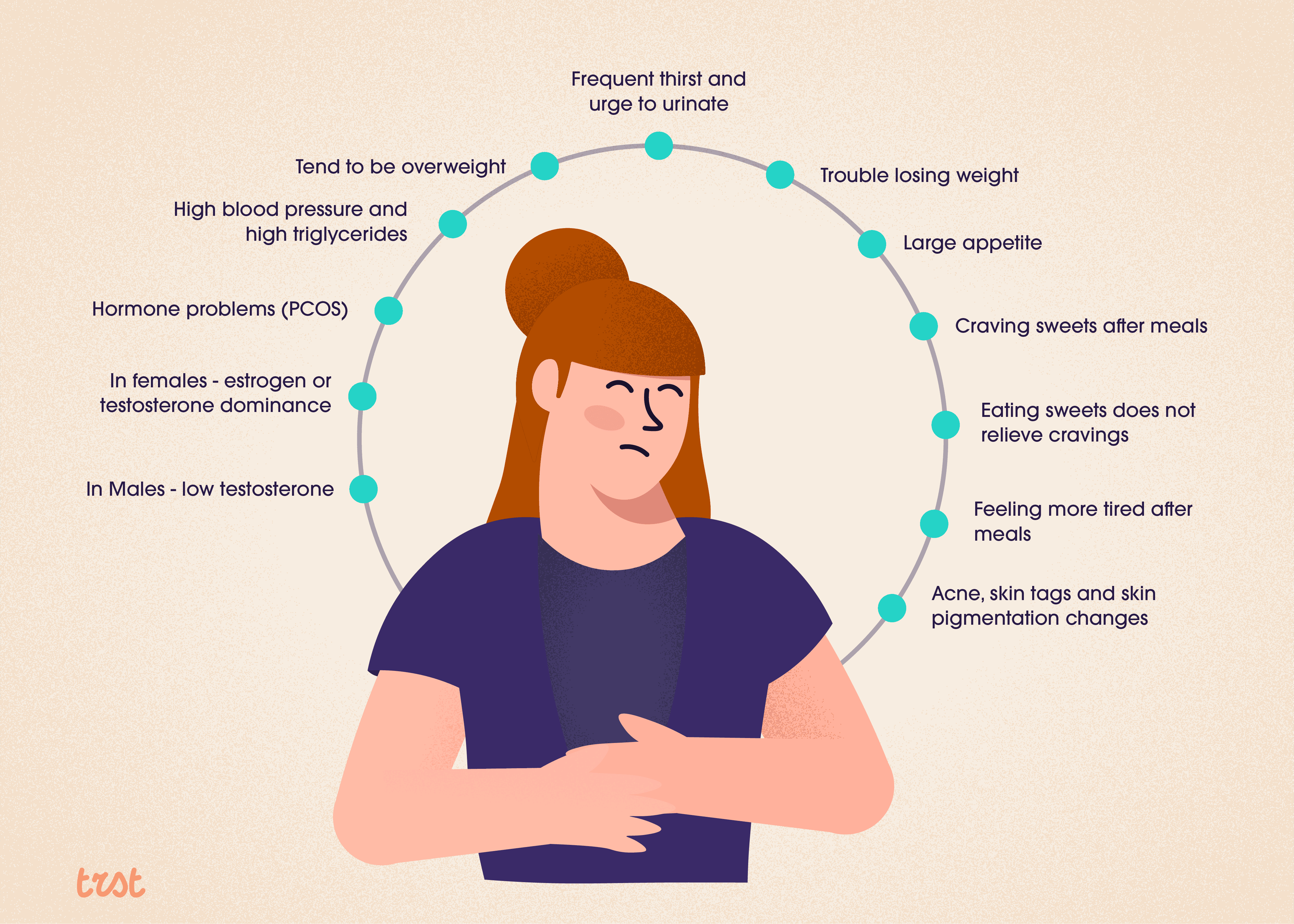
Other common signs are -
Fatigue: Feeling tired, especially after meals
Increased hunger: Craving food, particularly carbs.
Brain Fog: Having difficulty concentrating or trouble focusing.
Dark Patches of skin: Known as Acanthosis nigricans, appear on the neck, armpits, or groin.
Weight gain: Especially around the abdomen.
High blood pressure: Often associated with insulin resistance.
It is important to note that, many of us do not experience noticeable symptoms in the early stages. It is advised to get regular check-ups and blood tests for early detection. If you are experiencing any of these symptoms or have risk factors, consult your healthcare provider.
How To Diagnose Insulin Resistance?
There are multiple ways to diagnose insulin resistance. Your doctor will ask you about your symptoms, family history, and lifestyle. They’ll also check your weight, and blood pressure, and look for physical signs like acanthosis nigricans. Here are some of the tests that help in diagnosing insulin resistance -
HbA1c test
The A1c test is one way to diagnose insulin resistance, prediabetes, and diabetes. This test measures the average of your blood sugar over the previous 2 to 3 months.
Generally classified here are what the results mean:
An HbA1c under 5.7 % is considered normal
An HbA1c between 5.8 to 6.4% is considered prediabetic
An HbA1c equal to or above 6.5% is diagnosed as diabetes.
You’ll need your doctor to reconfirm the results. However, depending on the lab you have chosen for the test, the numbers could vary by 0.1% to 0.2%.
Fasting Glucose Test
This test shows your fasting blood sugar levels. For this test, you are required to fast (not eat or drink anything) for at least 8 hours. Your Doctor will be able to make a diagnosis for prediabetes or diabetes using this test.
Generally, here is what the results mean:
Fasting blood sugar levels under 10mg/dL is considered normal
Levels between 100 and 125 mg/dL are diagnostic for prediabetes
Levels equal to or greater than 126 mg/dL are diagnostic for diabetes.
Depending on the lab, these numbers can vary up to 3 mg/dL points in the cutoff numbers.
Glucose Tolerance Testing
A 2-hour glucose tolerance test is another way of diagnosing prediabetes or diabetes. Your blood glucose levels are taken before the test after which you will be given a premeasured sugar drink, and your blood glucose levels are checked again in 2 hours.
Generally, here’s what the results mean:
A blood glucose level under 140 mg/dL after 2 hours is considered normal.
A blood glucose level between 140 and 199 mg/dL is considered prediabetes.
A blood glucose level of 200 mg/dL or higher is considered diabetes.
Random Blood draws
Random blood sugar tests are useful if you are experiencing significant diabetes symptoms. However, the ADA ( American Diabetes Association) does not recommend random blood glucose tests for routine diabetes screening or the identification of pre-diabetes.
In Addition to all these tests, your doctor may also check your cholesterol levels, as insulin resistance often occurs alongside dyslipidemia (a metabolic disorder that occurs when there are abnormally high or low levels of lipids or lipoproteins in the blood.)
What are the Risks of Ignoring Insulin Resistance?
Insulin resistance if ignored can lead to a lot of serious health complications like -
Type 2 Diabetes - Insulin resistance is a known precursor to type 2 diabetes and without intervention, you have a higher chance of developing diabetes in the next 10 years.
Cardiovascular Diseases - Insulin resistance is associated with a higher risk of heart disease, and stroke due to its effects on blood pressure, cholesterol levels, and inflammation.
Polycystic Ovary Syndrome (PCOS/PCOD) - Insulin resistance can heighten hormonal imbalance in women.
Non-Alcoholic Fatty Liver Disease - With insulin resistance, and the body not being able to process excess glucose, it deposits as a fat layer on the liver causing fatty liver.
Metabolic Syndrome - A cluster of conditions like high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels are also associated with insulin resistance.
Early intervention and management are very crucial in preventing serious health risks.
Can Insulin Resistance Be Prevented?
While insulin resistance can be prevented in some cases, the genetic risk factors can’t be changed but there is good news! Many strategies can help prevent insulin resistance:
Living a healthy lifestyle: Adopting a healthy lifestyle is the cornerstone of prevention. This means maintaining a healthy weight, eating a balanced diet, and staying physically active.
Balanced Diet: Focus on whole foods, lean proteins, healthy fats, and complex carbohydrates.
Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise per week.
Healthy weight: Keep your BMI within the healthy range.
Limit alcohol and Quit Smoking: Alcohol and smoking can contribute to insulin resistance.
Monitoring risk factors: Regular check-ups and blood tests can help identify early signs of insulin resistance. If you have risk factors like a family history of diabetes or obesity, more frequent monitoring may be recommended.
How can Insulin Resistance Be Managed or Reversed?
The answer to this is yes it can be managed or reversed. Managing the condition often involves lifestyle changes and in some cases medication:
Dietary Changes
Low-carb diets: Reducing carb intake, especially refined carbs, can improve insulin sensitivity.
Increased Fiber: A high-fiber diet helps regulate blood sugar levels.
Reducing sugar intake: Limit added sugar and sweetened beverages.
Healthy fats: Incorporate sources of omega-3 fatty acids and monounsaturated fats.
Exercise
Aerobic exercise: Regular cardio activities like walking, swimming, or cycling.
Resistance training: Strength training helps build muscle, which improves insulin sensitivity.
High-intensity interval training (HIIT) can be particularly effective for improving insulin function.
Medication and Supplements
Metformin: A common medication that can improve insulin sensitivity.
Omega-3 Fatty acids: These may help you reduce inflammation and improve insulin function.
Berberine: A supplement that has shown promise in improving insulin sensitivity.
Lifestyle Modification
Stress reduction: Practice meditation, yoga, or deep breathing exercises to help with stress.
Sleep!: Aim for 7-9 hours of quality sleep a night to help with insulin resistance.
Weight Loss: Modest weight loss can significantly improve insulin sensitivity.
Conclusion
Insulin resistance is a serious condition that leads to significant health complications if left unmanaged. However, with early detection and appropriate lifestyle changes, it is possible to improve, manage and reverse insulin resistance.
Table Of Contents
Table Of Contents
Table Of Contents
Read More


Nov 6, 2024
Sayfali Rawlani
Sep 20, 2024
Sayfali Rawlani



Company
Copyright © 2025 trst health. All right reserved.
