What is Diabetes?
Jan 14, 2024
Ashima Raizada



Table Of Contents
Ever noticed how common diabetes has become? It's not just a senior citizen disease anymore. Over 537 million people globally are dealing with it, that's 1 in 10 adults! And brace yourself, experts predict this number will skyrocket to 1.3 billion by 2050. So, let's talk about what this condition really means and, more importantly, how we can tackle it. Welcome to your journey of diabetes education! (1)(2)
Highlights
Diabetes comes in different types - Type 1, Type 2, and gestational during pregnancy, each with its unique characteristics.
Recognise symptoms like excessive hunger, fatigue, and blurred vision, and understand risk factors such as family history, obesity, and inactivity.
Diabetes can lead to serious complications, including eye problems, foot complications, heart issues, kidney disease, and nerve damage.
Blood tests like HbA1C, random blood sugar, fasting blood sugar, and glucose tolerance tests can help in diagnosis of diabetes.
Lifestyle adjustments, like a balanced diet, regular exercise, weight control, and stress management, play a key role. CGMs and diabetes education are an important part of your journey.
Insulin Resistance: The Precursor
Diabetes kicks off with elevated blood sugar levels, often due to insulin resistance. Imagine insulin as the key that unlocks cells to let glucose in and fuel the body. But with insulin resistance, cells in muscles, liver, and fat become stubborn, disregarding insulin's cue. This resistance prevents glucose absorption, leaving excess sugar circulating in the bloodstream. In a nutshell, diabetes occurs when insulin faces resistance, disrupting its vital role in regulating blood sugar levels.
What are the types of diabetes?
There are many types of diabetes but here are the 3 main ones:
Type 1 diabetes
In this case, your body is unable to produce sufficient insulin, leading to the accumulation of glucose in your bloodstream. It is believed to be an autoimmune disease. Those diagnosed with Type 1 diabetes need insulin injections to deal with blood sugar.
Type 2 diabetes
This phase usually begins with insulin resistance. In simple terms, when your body struggles to use insulin effectively, it prompts the pancreas to work overtime, producing more insulin. However, this increased demand eventually surpasses the pancreas's capacity. Consequently, insulin production drops, leading to elevated blood sugar levels.
Gestational diabetes
Insulin-blocking hormones produced during pregnancy lead to gestational diabetes. This specific type occurs solely during pregnancy and tends to be more prevalent in individuals with preexisting prediabetes or a family history of diabetes. Interestingly, approximately half of those diagnosed with gestational diabetes later develop type 2 diabetes. (3)
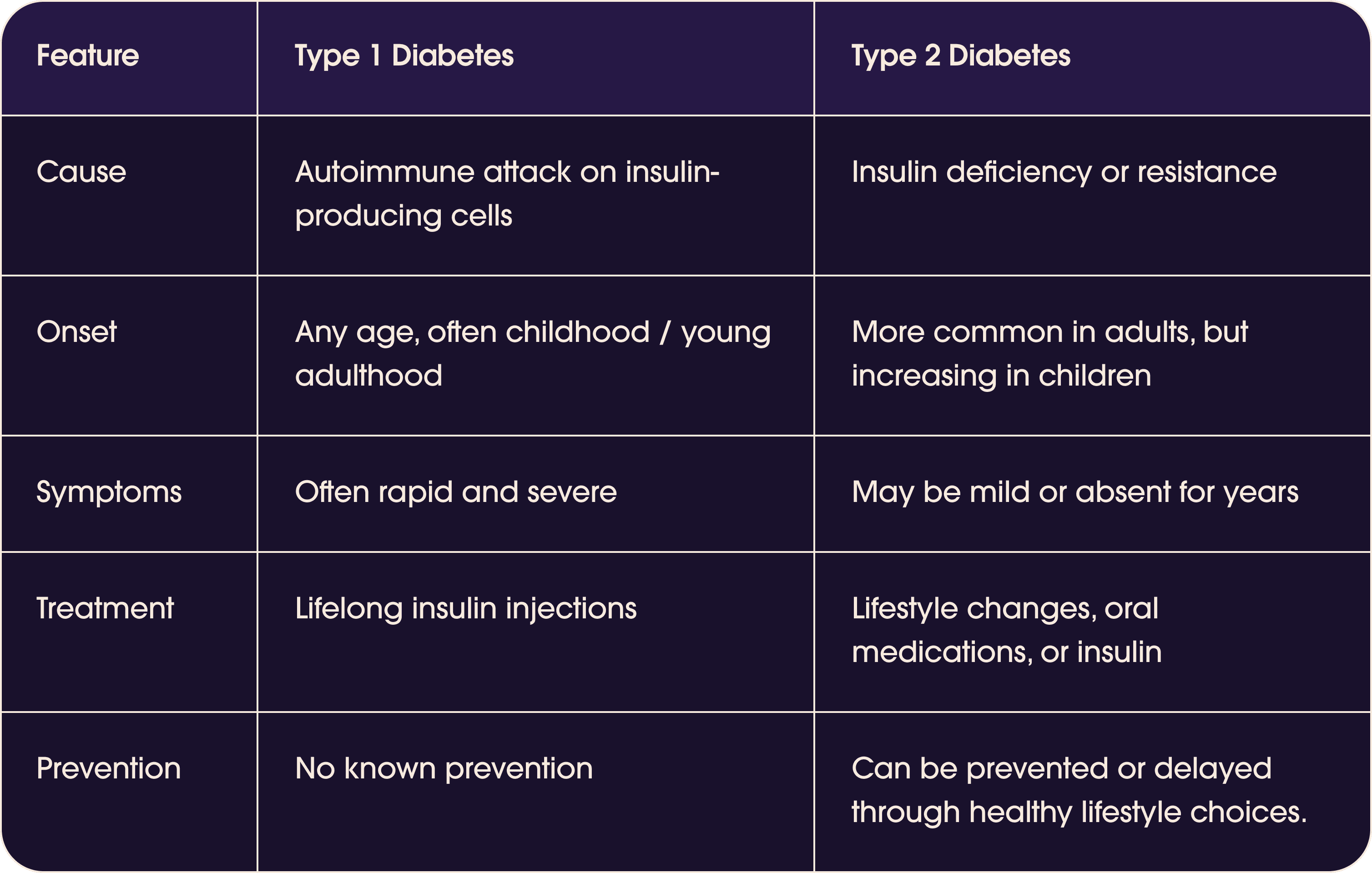
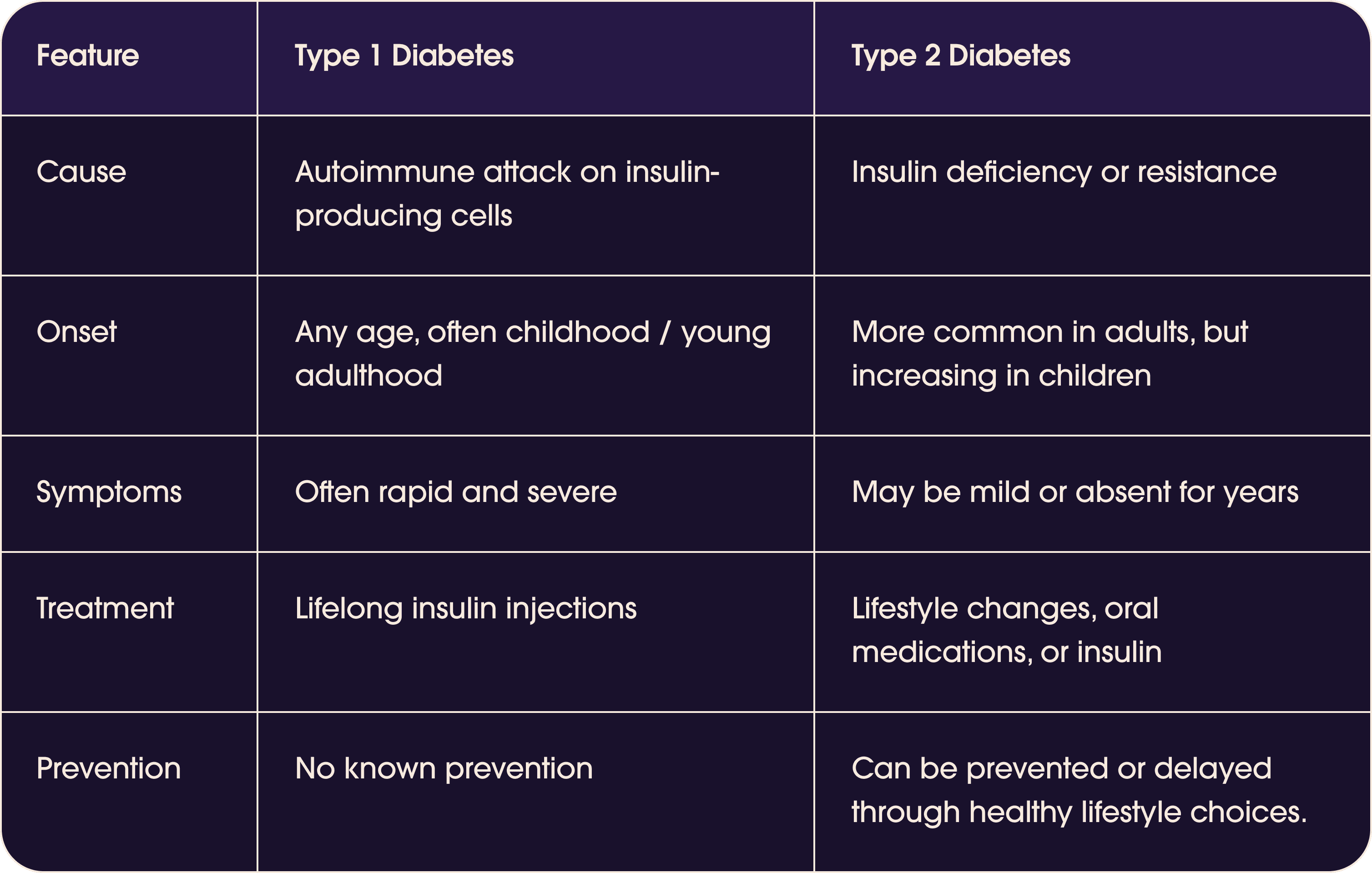
Both type 1 and type 2 diabetes are chronic conditions that affect how your body regulates blood sugar (glucose). However, they have different causes, symptoms, and treatments.
Difference between Type 1 and Type 2 diabetes
And then there is also prediabetes, a precursor to diabetes. Prediabetes, where your sugar levels are creeping up, but not enough to be full-blown diabetes yet. (4)
Symptoms of Diabetes
While excessive thirst and bathroom breaks are classic signs, diabetes can be a sneaky condition. Sometimes it can give you signs but sometimes it gives no signs at all! Here's what you need to watch out for:
Increased hunger and fatigue: your body's not getting the fuel it needs!
Blurred vision: sugar messing with your eyes
Slow-healing wounds: sugar can slow down your body's repair ability
Unexplained weight loss: your body starts burning muscle for energy
Darkened skin patches: specially in the groin, neck and armpits
Skin and other infections
Extremely dry skin
Numbness or tingling in hands or feet (5)
These are just some clues, so if you're experiencing any of them, don't hesitate to chat with your doctor. Early diagnosis is always good for further disease progression.
Who's at Risk?
Anyone can get diabetes, but some folks have a higher propensity, like:
People with family history of diabetes (genetics, gotta love 'em)
Folks who are overweight or obese
Physically inactive individuals (your body needs to move that sugar around!)
Certain ethnicities (not fair, but research is helping us understand why) (6)
Men with a waist circumference exceeding 40 inches and non-pregnant women with a waist circumference above 35 inches. (7)
Additionally, the American Diabetes Association (ADA) recommends the following people get screened for diabetes:
Anyone with a BMI over 25 (23 for Asian Americans) with additional risk factors
Individuals over 35 should have an initial blood sugar screening, repeated every three years if normal. Particularly those with a poor lifestyle.
Women with gestational diabetes should be screened every three years.
People who have been diagnosed with prediabetes should get tested annually
People who have HIV (8)
Consequences of Diabetes
Unchecked diabetes can lead to some scary serious complications, like:
There are long-term issues that can creep up gradually, causing serious trouble if you don't stay on top of them.
Eye problems (Diabetic Retinopathy)
There's a risk of developing diabetic retinopathy which messes with your eyesight. But here's the thing - catch it early through eye screening, and you can get treatment to prevent losing your vision.
Foot problems
Diabetes means serious foot business. Nerve damage messes with how your feet feel, and high blood sugar makes it harder for cuts and sores to heal. Don't ignore any changes in how your feet look or feel - tell your GP pronto.
Heart attack and stroke
High blood sugar levels can mess with your blood vessels over time, possibly leading to heart attacks and strokes.
Kidney problems (nephropathy)
High blood sugar can be tough on your kidneys in the long run, making it harder for them to clear out extra stuff. High blood sugar and pressure team up to cause what's called diabetic nephropathy or kidney disease.
Nerve damage (neuropathy)
High blood sugar levels can lead to nerve damage, messing with how your nerves send messages throughout your body. It can affect your vision, hearing, sensation, and movement.
Gum disease and other oral problems
Too much sugar in your blood can cause trouble for your teeth and gums. Bacteria love the sugar, producing acid that damages your enamel. Your gums can also take a hit, making infections more likely.
Cancer and related conditions
If you've got consistently high blood sugar, your odds of certain cancers go up. And watch out - some cancer treatments might mess with your diabetes and make blood sugar control tougher.
Sexual dysfunctions in women
Blood vessels and nerves can take a hit, limiting blood flow to your sexual organs. This might mean less sensation, and you're also more prone to thrush or urinary tract infections.
Sexual dysfunctions in men
Restricted blood flow might cause trouble getting in the mood and lead to erectile dysfunction, which is just another way of saying difficulty getting and staying, well, you know. (9)(10)With proper management, you can live a long, healthy life, even with diabetes.
Diabetes Diagnosis
Know that diagnosing diabetes usually involves blood tests and monitoring your sugar levels. Your doctor may ask you to get specific tests to diagnose your diabetes:
HbA1C Test: This blood test provides a snapshot of your average blood sugar level over the past 2 to 3 months without requiring fasting. It gauges the percentage of blood sugar attached to hemoglobin, a protein in red blood cells that carries oxygen. A level of 6.5% or higher on two separate tests indicates diabetes, while 5.7% to 6.4% suggests prediabetes, and below 5.7% is considered normal.
Random Blood Sugar Test: This test, taken at any time, reveals diabetes if the blood sugar level is 200 mg/dL (11.1 mmol/L) or higher, regardless of when you last ate.
Fasting Blood Sugar Test: Conducted after an overnight fast, a level below 100 mg/dL (5.6 mmol/L) is normal, 100 to 125 mg/dL (5.6 to 6.9 mmol/L) indicates prediabetes, and 126 mg/dL (7 mmol/L) or higher on two separate tests signifies diabetes.
Glucose Tolerance Test: After an overnight fast, this test involves measuring fasting blood sugar, followed by drinking a sugary solution with blood sugar monitoring for the next two hours. A blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal, over 200 mg/dL (11.1 mmol/L) after two hours indicates diabetes and 140 to 199 mg/dL (7.8 mmol/L to 11.0 mmol/L) points to prediabetes. (8)
Diabetes Prevention & Treatment
While each person deals with this disease differently, some common treatments can help you live well despite high blood sugar levels. Obviously the first step is getting the right education on diabetes so you can know what to expect. Treatment plans vary depending on your type and severity, but they often include lifestyle changes such as:
Prioritizing Fiber and Protein: Emphasize fiber-rich foods like vegetables and protein sources such as eggs and fish to regulate blood sugar.
Ditching Calorie Counting: Shift focus to nutrients - fiber, proteins, and carbs - over calorie counting to manage glucose, insulin, and weight effectively.
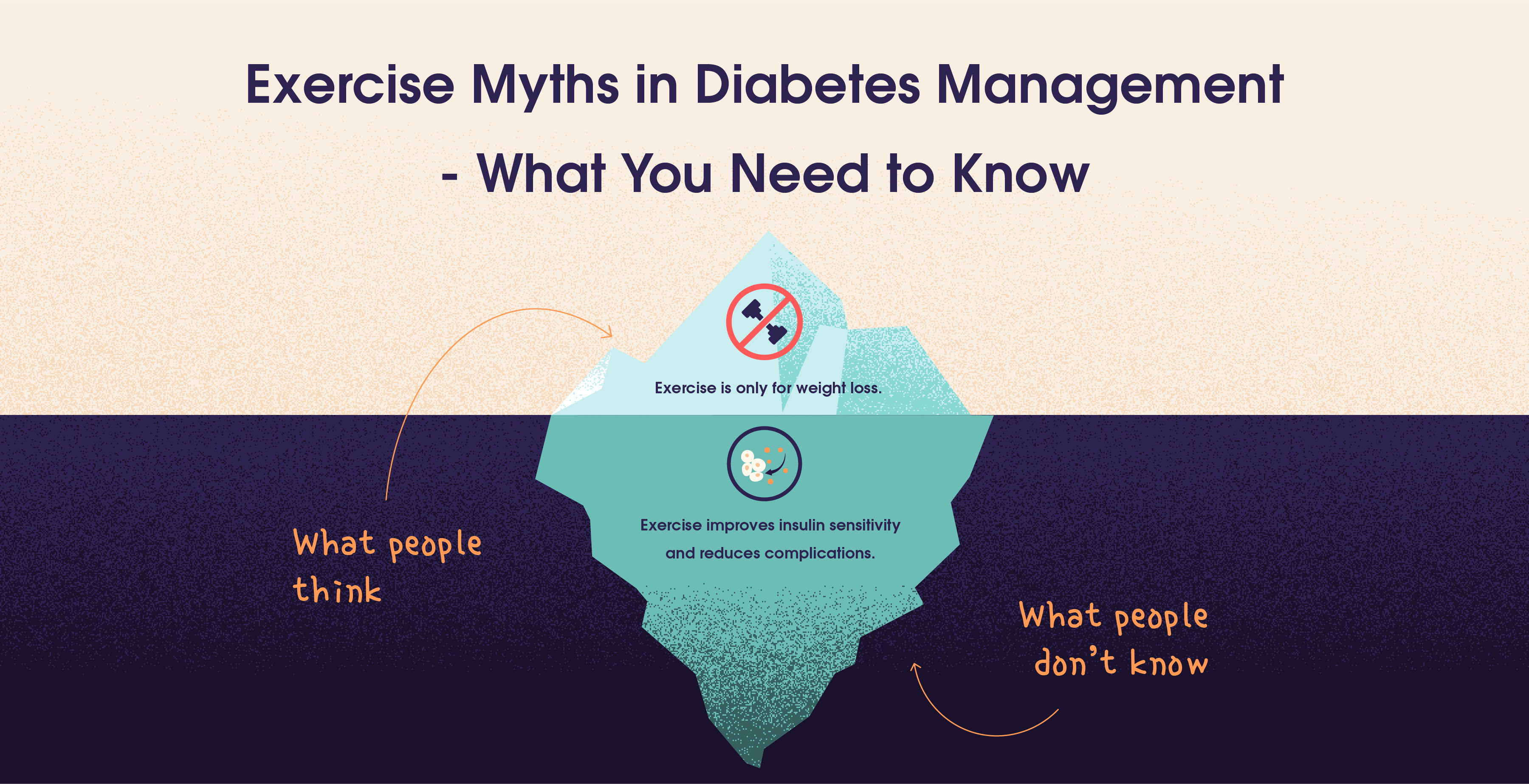
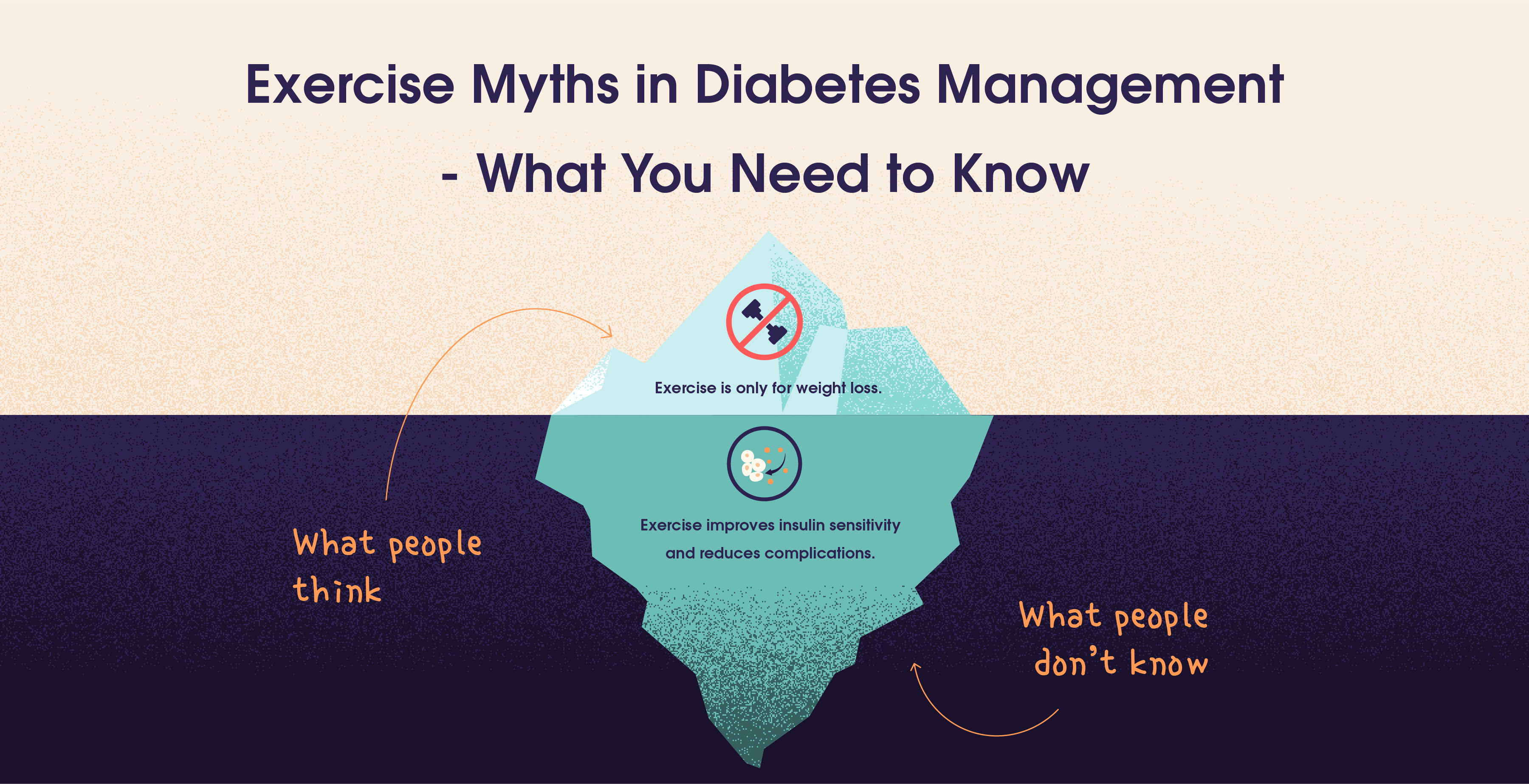
Exercising Regularly: Combine strength training with enjoyable aerobic activities to efficiently use glucose and support weight management.
Sequence Meals: Start meals with fiber, followed by protein and fats, and then carbs and sugars to slow down glucose absorption, leading to lower glucose levels. (11)
Trying Intermittent Fasting: Sync eating with your body's natural rhythm, aiming for a 12-16 hour fasting window, potentially lowering insulin resistance. Research from the American Heart Association shows that intermittent fasting along with lifestyle habits, circadian rhythm changes and gut microbiome improvement can potentially lower insulin resistance. (12)
Regulating Circadian Rhythm: Prioritize quality sleep, morning sunlight exposure, and a light dinner to support a balanced circadian rhythm.
Managing Stress: Incorporate stress-relief practices like meditation and deep breathing into your routine to lower cortisol levels.
Managing Weight: Achieve and maintain a healthy weight to improve insulin sensitivity and manage high blood sugar. Studies show that losing 5% of your body weight can improve insulin sensitivity. (13)
Limiting Alcohol Intake: Stick to one drink a day to reduce the risk of complications associated with diabetes.
Quitting Smoking: Ditching cigarettes significantly lowers the risk of diabetes-related complications.
Stay Hydrated: Increase water intake to help regulate blood sugar levels and overall health.
Consult Your Healthcare Team: Maintain open communication with healthcare professionals, explore diabetes management programs such as Trst's Urth app, and consider medications if needed. 
Most often, treatment and prevention are the same because doing all of the above also accounts for reducing blood sugar spikes and insulin resistance.
Self-Testing In Diabetes: Using CGM's
When your blood sugar is constantly high, it's always advisable to constantly monitor it. You can use a Continuous Glucose Monitor (CGM) for real-time data or a blood sugar meter (glucometer) at home with a small blood drop. CGMs provide real-time information about blood glucose levels, offering convenience and continuous monitoring. Testing helps:
Monitor Medications: Check how well your medications are working.
Detect Levels: Identify high or low blood sugar levels promptly.
Track Progress: Assess your progress towards treatment goals set by your healthcare provider.
Understand Impact: Learn how diet and exercise influence blood sugar levels.
Recognize Factors: Understand how external factors like illness or stress affect blood sugar.
The frequency of testing depends on your diabetes type and treatment plan advised by your healthcare provider. It's a straightforward way to manage it effectively and maintain overall health.
The Crucial Role of Diabetes Education
We believe that knowledge is a powerful tool for any disease. Diabetes education isn't just about learning facts and figures; it's about unlocking knowledge, confidence and a support system to actively manage your health and well-being. Care-givers, diabetics and basically everyone should have access to diabetes education. It's the key to taking control, making informed choices, and navigating the complexities of diabetes every day. Diabetes education gives you:
Understanding the Condition: Diabetes education helps individuals understand the nature of their condition, its causes, and its impact on their health. This knowledge is essential for managing the disease effectively.
Self-Management Skills: Education provides practical skills for self-management, including monitoring blood glucose levels, administering insulin (if necessary), and managing medications. This empowers individuals to take an active role in their care.
Nutritional Guidance: Diabetes education offers guidance on healthy eating, meal planning, and understanding the effects of different foods on blood sugar levels. This is crucial for maintaining optimal blood glucose control.
Physical Activity: Learning about the importance of regular physical activity and its role in blood sugar management helps individuals incorporate exercise into their routine safely.
Medication Management: Understanding the purpose, dosage, and timing of medications helps individuals adhere to their treatment plan, reducing the risk of complications.
Prevention of Complications: Diabetes education provides information on preventing complications such as neuropathy, retinopathy, and cardiovascular issues through proper management and lifestyle choices.
Psychosocial Support: Living with diabetes can be emotionally challenging. Diabetes education often includes psychosocial support to help individuals cope with stress, anxiety, and other emotional aspects of the condition.
Take a look at our diabetes education page to get all your questions answered.
Conclusion
Diabetes, a prevalent health concern affecting millions globally, involves elevated blood sugar levels. Whether it's due to insufficient insulin production (Type 1) or resistance to insulin's effects (Type 2), early detection and proactive management are crucial. Symptoms vary, from increased thirst to slow healing, and risk factors include family history and lifestyle choices. Complications, ranging from eye problems to kidney issues, highlight the importance of vigilant care. Managing it involves lifestyle adjustments, regular monitoring using tools like Continuous Glucose Monitors, and education for informed decision-making. Despite its challenges, with the right knowledge and support, individuals can lead healthy lives while managing diabetes effectively.
Resources
Global diabetes cases expected to soar from 529 million to 1.3 billion by 2050
More Than 1.3 Billion People Worldwide Predicted to Have Diabetes by 2050
Food Order Has a Significant Impact on Postprandial Glucose and Insulin Levels - PMC
Standards of Medical Care in Diabetes - 2022 Abridged for Primary Care Providers
Ever noticed how common diabetes has become? It's not just a senior citizen disease anymore. Over 537 million people globally are dealing with it, that's 1 in 10 adults! And brace yourself, experts predict this number will skyrocket to 1.3 billion by 2050. So, let's talk about what this condition really means and, more importantly, how we can tackle it. Welcome to your journey of diabetes education! (1)(2)
Highlights
Diabetes comes in different types - Type 1, Type 2, and gestational during pregnancy, each with its unique characteristics.
Recognise symptoms like excessive hunger, fatigue, and blurred vision, and understand risk factors such as family history, obesity, and inactivity.
Diabetes can lead to serious complications, including eye problems, foot complications, heart issues, kidney disease, and nerve damage.
Blood tests like HbA1C, random blood sugar, fasting blood sugar, and glucose tolerance tests can help in diagnosis of diabetes.
Lifestyle adjustments, like a balanced diet, regular exercise, weight control, and stress management, play a key role. CGMs and diabetes education are an important part of your journey.
Insulin Resistance: The Precursor
Diabetes kicks off with elevated blood sugar levels, often due to insulin resistance. Imagine insulin as the key that unlocks cells to let glucose in and fuel the body. But with insulin resistance, cells in muscles, liver, and fat become stubborn, disregarding insulin's cue. This resistance prevents glucose absorption, leaving excess sugar circulating in the bloodstream. In a nutshell, diabetes occurs when insulin faces resistance, disrupting its vital role in regulating blood sugar levels.
What are the types of diabetes?
There are many types of diabetes but here are the 3 main ones:
Type 1 diabetes
In this case, your body is unable to produce sufficient insulin, leading to the accumulation of glucose in your bloodstream. It is believed to be an autoimmune disease. Those diagnosed with Type 1 diabetes need insulin injections to deal with blood sugar.
Type 2 diabetes
This phase usually begins with insulin resistance. In simple terms, when your body struggles to use insulin effectively, it prompts the pancreas to work overtime, producing more insulin. However, this increased demand eventually surpasses the pancreas's capacity. Consequently, insulin production drops, leading to elevated blood sugar levels.
Gestational diabetes
Insulin-blocking hormones produced during pregnancy lead to gestational diabetes. This specific type occurs solely during pregnancy and tends to be more prevalent in individuals with preexisting prediabetes or a family history of diabetes. Interestingly, approximately half of those diagnosed with gestational diabetes later develop type 2 diabetes. (3)
Both type 1 and type 2 diabetes are chronic conditions that affect how your body regulates blood sugar (glucose). However, they have different causes, symptoms, and treatments.
Difference between Type 1 and Type 2 diabetes
And then there is also prediabetes, a precursor to diabetes. Prediabetes, where your sugar levels are creeping up, but not enough to be full-blown diabetes yet. (4)
Symptoms of Diabetes
While excessive thirst and bathroom breaks are classic signs, diabetes can be a sneaky condition. Sometimes it can give you signs but sometimes it gives no signs at all! Here's what you need to watch out for:
Increased hunger and fatigue: your body's not getting the fuel it needs!
Blurred vision: sugar messing with your eyes
Slow-healing wounds: sugar can slow down your body's repair ability
Unexplained weight loss: your body starts burning muscle for energy
Darkened skin patches: specially in the groin, neck and armpits
Skin and other infections
Extremely dry skin
Numbness or tingling in hands or feet (5)
These are just some clues, so if you're experiencing any of them, don't hesitate to chat with your doctor. Early diagnosis is always good for further disease progression.
Who's at Risk?
Anyone can get diabetes, but some folks have a higher propensity, like:
People with family history of diabetes (genetics, gotta love 'em)
Folks who are overweight or obese
Physically inactive individuals (your body needs to move that sugar around!)
Certain ethnicities (not fair, but research is helping us understand why) (6)
Men with a waist circumference exceeding 40 inches and non-pregnant women with a waist circumference above 35 inches. (7)
Additionally, the American Diabetes Association (ADA) recommends the following people get screened for diabetes:
Anyone with a BMI over 25 (23 for Asian Americans) with additional risk factors
Individuals over 35 should have an initial blood sugar screening, repeated every three years if normal. Particularly those with a poor lifestyle.
Women with gestational diabetes should be screened every three years.
People who have been diagnosed with prediabetes should get tested annually
People who have HIV (8)
Consequences of Diabetes
Unchecked diabetes can lead to some scary serious complications, like:
There are long-term issues that can creep up gradually, causing serious trouble if you don't stay on top of them.
Eye problems (Diabetic Retinopathy)
There's a risk of developing diabetic retinopathy which messes with your eyesight. But here's the thing - catch it early through eye screening, and you can get treatment to prevent losing your vision.
Foot problems
Diabetes means serious foot business. Nerve damage messes with how your feet feel, and high blood sugar makes it harder for cuts and sores to heal. Don't ignore any changes in how your feet look or feel - tell your GP pronto.
Heart attack and stroke
High blood sugar levels can mess with your blood vessels over time, possibly leading to heart attacks and strokes.
Kidney problems (nephropathy)
High blood sugar can be tough on your kidneys in the long run, making it harder for them to clear out extra stuff. High blood sugar and pressure team up to cause what's called diabetic nephropathy or kidney disease.
Nerve damage (neuropathy)
High blood sugar levels can lead to nerve damage, messing with how your nerves send messages throughout your body. It can affect your vision, hearing, sensation, and movement.
Gum disease and other oral problems
Too much sugar in your blood can cause trouble for your teeth and gums. Bacteria love the sugar, producing acid that damages your enamel. Your gums can also take a hit, making infections more likely.
Cancer and related conditions
If you've got consistently high blood sugar, your odds of certain cancers go up. And watch out - some cancer treatments might mess with your diabetes and make blood sugar control tougher.
Sexual dysfunctions in women
Blood vessels and nerves can take a hit, limiting blood flow to your sexual organs. This might mean less sensation, and you're also more prone to thrush or urinary tract infections.
Sexual dysfunctions in men
Restricted blood flow might cause trouble getting in the mood and lead to erectile dysfunction, which is just another way of saying difficulty getting and staying, well, you know. (9)(10)With proper management, you can live a long, healthy life, even with diabetes.
Diabetes Diagnosis
Know that diagnosing diabetes usually involves blood tests and monitoring your sugar levels. Your doctor may ask you to get specific tests to diagnose your diabetes:
HbA1C Test: This blood test provides a snapshot of your average blood sugar level over the past 2 to 3 months without requiring fasting. It gauges the percentage of blood sugar attached to hemoglobin, a protein in red blood cells that carries oxygen. A level of 6.5% or higher on two separate tests indicates diabetes, while 5.7% to 6.4% suggests prediabetes, and below 5.7% is considered normal.
Random Blood Sugar Test: This test, taken at any time, reveals diabetes if the blood sugar level is 200 mg/dL (11.1 mmol/L) or higher, regardless of when you last ate.
Fasting Blood Sugar Test: Conducted after an overnight fast, a level below 100 mg/dL (5.6 mmol/L) is normal, 100 to 125 mg/dL (5.6 to 6.9 mmol/L) indicates prediabetes, and 126 mg/dL (7 mmol/L) or higher on two separate tests signifies diabetes.
Glucose Tolerance Test: After an overnight fast, this test involves measuring fasting blood sugar, followed by drinking a sugary solution with blood sugar monitoring for the next two hours. A blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal, over 200 mg/dL (11.1 mmol/L) after two hours indicates diabetes and 140 to 199 mg/dL (7.8 mmol/L to 11.0 mmol/L) points to prediabetes. (8)
Diabetes Prevention & Treatment
While each person deals with this disease differently, some common treatments can help you live well despite high blood sugar levels. Obviously the first step is getting the right education on diabetes so you can know what to expect. Treatment plans vary depending on your type and severity, but they often include lifestyle changes such as:
Prioritizing Fiber and Protein: Emphasize fiber-rich foods like vegetables and protein sources such as eggs and fish to regulate blood sugar.
Ditching Calorie Counting: Shift focus to nutrients - fiber, proteins, and carbs - over calorie counting to manage glucose, insulin, and weight effectively.
Exercising Regularly: Combine strength training with enjoyable aerobic activities to efficiently use glucose and support weight management.
Sequence Meals: Start meals with fiber, followed by protein and fats, and then carbs and sugars to slow down glucose absorption, leading to lower glucose levels. (11)
Trying Intermittent Fasting: Sync eating with your body's natural rhythm, aiming for a 12-16 hour fasting window, potentially lowering insulin resistance. Research from the American Heart Association shows that intermittent fasting along with lifestyle habits, circadian rhythm changes and gut microbiome improvement can potentially lower insulin resistance. (12)
Regulating Circadian Rhythm: Prioritize quality sleep, morning sunlight exposure, and a light dinner to support a balanced circadian rhythm.
Managing Stress: Incorporate stress-relief practices like meditation and deep breathing into your routine to lower cortisol levels.
Managing Weight: Achieve and maintain a healthy weight to improve insulin sensitivity and manage high blood sugar. Studies show that losing 5% of your body weight can improve insulin sensitivity. (13)
Limiting Alcohol Intake: Stick to one drink a day to reduce the risk of complications associated with diabetes.
Quitting Smoking: Ditching cigarettes significantly lowers the risk of diabetes-related complications.
Stay Hydrated: Increase water intake to help regulate blood sugar levels and overall health.
Consult Your Healthcare Team: Maintain open communication with healthcare professionals, explore diabetes management programs such as Trst's Urth app, and consider medications if needed. 
Most often, treatment and prevention are the same because doing all of the above also accounts for reducing blood sugar spikes and insulin resistance.
Self-Testing In Diabetes: Using CGM's
When your blood sugar is constantly high, it's always advisable to constantly monitor it. You can use a Continuous Glucose Monitor (CGM) for real-time data or a blood sugar meter (glucometer) at home with a small blood drop. CGMs provide real-time information about blood glucose levels, offering convenience and continuous monitoring. Testing helps:
Monitor Medications: Check how well your medications are working.
Detect Levels: Identify high or low blood sugar levels promptly.
Track Progress: Assess your progress towards treatment goals set by your healthcare provider.
Understand Impact: Learn how diet and exercise influence blood sugar levels.
Recognize Factors: Understand how external factors like illness or stress affect blood sugar.
The frequency of testing depends on your diabetes type and treatment plan advised by your healthcare provider. It's a straightforward way to manage it effectively and maintain overall health.
The Crucial Role of Diabetes Education
We believe that knowledge is a powerful tool for any disease. Diabetes education isn't just about learning facts and figures; it's about unlocking knowledge, confidence and a support system to actively manage your health and well-being. Care-givers, diabetics and basically everyone should have access to diabetes education. It's the key to taking control, making informed choices, and navigating the complexities of diabetes every day. Diabetes education gives you:
Understanding the Condition: Diabetes education helps individuals understand the nature of their condition, its causes, and its impact on their health. This knowledge is essential for managing the disease effectively.
Self-Management Skills: Education provides practical skills for self-management, including monitoring blood glucose levels, administering insulin (if necessary), and managing medications. This empowers individuals to take an active role in their care.
Nutritional Guidance: Diabetes education offers guidance on healthy eating, meal planning, and understanding the effects of different foods on blood sugar levels. This is crucial for maintaining optimal blood glucose control.
Physical Activity: Learning about the importance of regular physical activity and its role in blood sugar management helps individuals incorporate exercise into their routine safely.
Medication Management: Understanding the purpose, dosage, and timing of medications helps individuals adhere to their treatment plan, reducing the risk of complications.
Prevention of Complications: Diabetes education provides information on preventing complications such as neuropathy, retinopathy, and cardiovascular issues through proper management and lifestyle choices.
Psychosocial Support: Living with diabetes can be emotionally challenging. Diabetes education often includes psychosocial support to help individuals cope with stress, anxiety, and other emotional aspects of the condition.
Take a look at our diabetes education page to get all your questions answered.
Conclusion
Diabetes, a prevalent health concern affecting millions globally, involves elevated blood sugar levels. Whether it's due to insufficient insulin production (Type 1) or resistance to insulin's effects (Type 2), early detection and proactive management are crucial. Symptoms vary, from increased thirst to slow healing, and risk factors include family history and lifestyle choices. Complications, ranging from eye problems to kidney issues, highlight the importance of vigilant care. Managing it involves lifestyle adjustments, regular monitoring using tools like Continuous Glucose Monitors, and education for informed decision-making. Despite its challenges, with the right knowledge and support, individuals can lead healthy lives while managing diabetes effectively.
Resources
Global diabetes cases expected to soar from 529 million to 1.3 billion by 2050
More Than 1.3 Billion People Worldwide Predicted to Have Diabetes by 2050
Food Order Has a Significant Impact on Postprandial Glucose and Insulin Levels - PMC
Standards of Medical Care in Diabetes - 2022 Abridged for Primary Care Providers
Table Of Contents
Table Of Contents
Table Of Contents
Read More


Apr 2, 2025
Sayfali Rawlani
Feb 17, 2025
Aparna Hurtis


Feb 10, 2025
Aparna Hurtis



Company
Copyright © 2025 trst health. All right reserved.